ABBOTT PARK, Ill., Nov. 17, 2014 - People aged 65 and older, who were being treated for chronic obstructive pulmonary disease (COPD) in the hospital and received nutrition treatment (oral nutrition supplements) had reduced lengths of stay, hospital costs and chances of returning to the hospital within 30-days, according to a study published in CHEST.
Chronic obstructive pulmonary disease (COPD) -- which includes conditions like chronic bronchitis and emphysema -- is a lung disease that compromises breathing. As COPD often occurs among seniors, it is one of the leading causes of disability and death in the U.S. and has been estimated to cost $50 billion per year.
Nutrition Treatment Shows Better Outcomes
The study, which was supported by Abbott, evaluated Medicare patients, 65 and older, who were hospitalized with a primary diagnosis of COPD. The study demonstrates that when older patients with COPD received nutrition treatment in the hospital, it reduced their length of stay by 1.88 days (21.5 percent) and total hospital costs by $1,570 (12.5 percent) on average, compared to those who did not receive nutrition treatment. When looking at the likelihood of readmission within 30 days, the people who received nutrition treatment had a 13.1 percent reduction in 30-day readmission.
"Our findings suggest that screening seniors in the hospital for malnutrition risk and providing cost-effective treatment for those who are malnourished or at risk, can have a positive health impact on outcomes," said Julia Thornton Snider, Ph.D., at Precision Health Economics and lead author for the study. "In addition, our new readmission data suggests economic benefits for the hospital, including how they may better achieve the new Medicare mandates for reducing readmission rates in elderly COPD patients."
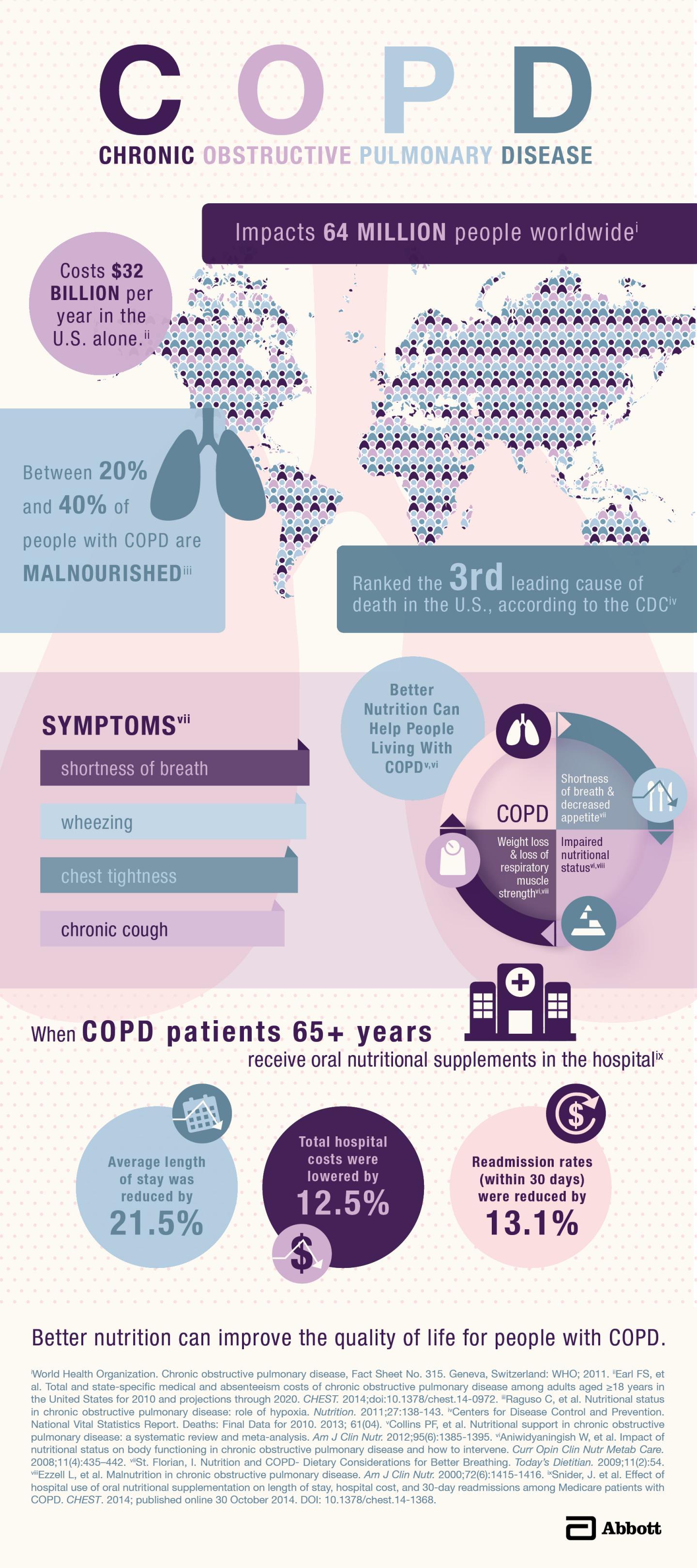
This image shows the impact of COPD in the United States.
(Photo Credit: Abbott)
This year, Medicare will raise its maximum penalty for hospitals that have too many patients readmitted within 30-days. The program, part of the Affordable Care Act, typically calculates this number by looking at readmissions of patients who had a heart attack, heart failure and pneumonia. Beginning in 2015 Medicare will examine readmissions of total hip/knee replacements and patients with COPD. Medicare patients with COPD already incur roughly $20,500 more in healthcare costs than those without.
Impact of Poor Nutrition on People with COPD
Those with COPD are at a higher risk of being malnourished, which can weaken their strength and immune system and cause complications during recovery. ,
Despite the nutritional need for people with COPD and the fact that it's the third leading cause of death in the U.S., current guidelines do not include any specific recommendations for addressing nutritional deficiencies in this group. However, researchers are working to change this as a growing number of studies are being published that show the economic and health benefits that nutrition screenings and treatment has on COPD as well as other health issues.
"Abbott has been partnering with leading research institutions to better understand how we can improve health outcomes of people affected by certain conditions," said Robert H. Miller, Ph.D., Divisional Vice President, R&D, Scientific and Medical Affairs, at Abbott Nutrition. "By identifying solutions, such as oral nutritional supplements, we may be able to help people with COPD have better health results and reduce healthcare costs."
Source: Fleishman-Hillard, Inc.