HOUSTON -- (May 5, 2014) -- A Rice University-led analysis of the metabolic profiles of hundreds of ovarian tumors has revealed a new test to determine whether ovarian cancer cells have the potential to metastasize, or spread to other parts of the body. The study also suggests how ovarian cancer treatments can be tailored based on the metabolic profile of a particular tumor.
The research, which appears online this week in Molecular Systems Biology, was conducted at the Texas Medical Center in Houston by researchers from Rice, the University of Texas MD Anderson Cancer Center and Baylor College of Medicine.
"We found a striking difference between the metabolic profiles of poorly aggressive and highly aggressive ovarian tumor cells, particularly with respect to their production and use of the amino acid glutamine," said lead researcher Deepak Nagrath of Rice. "For example, we found that highly aggressive ovarian cancer cells are glutamine-dependent, and in our laboratory studies, we showed that depriving such cells of external sources of glutamine -- as some experimental drugs do -- was an effective way to kill late-stage cells.
"The story for poorly aggressive cells was quite different," said Nagrath, assistant professor of chemical and biomolecular engineering and of bioengineering at Rice. "These cells use an internal metabolic pathway to produce a significant portion of the glutamine that they consume, so a different type of treatment -- one aimed toward internal glutamine sources -- will be needed to target cells of this type."
The research is part of a growing effort among cancer researchers worldwide to create treatments that target the altered metabolism of cancer cells. It has long been known that cancer cells adjust their metabolism in subtle ways that allow them to proliferate faster and survive better. In 1924, Otto Warburg showed that cancer cells produced far more energy from glycolysis than did normal cells. The Nobel Prize-winning discovery became known as the "Warburg effect," and researchers long believed that all cancers behaved in this way. Intense research in recent decades has revealed a more nuanced picture.
"Each type of cancer appears to have its own metabolic signature," Nagrath said. "For instance, kidney cancer does not rely on glutamine, and though breast cancer gets some of its energy from glutamine, it gets even more from glycolysis. For other cancers, including glioblastoma and pancreatic cancer, glutamine appears to be the primary energy source."
Nagrath, director of Rice's Laboratory for Systems Biology of Human Diseases, said the new metabolic analysis indicates that ovarian cancer may be susceptible to multidrug cocktails, particularly if the amounts of the drugs can be tailored to match the metabolic profile of a patient's tumor.
The research also revealed a specific biochemical test that pathologists could use to guide such treatments. The test involves measuring the ratio between the amount of glutamine that a cell takes up from outside and the amount of glutamine it makes internally.
This is Deepak Nagrath.
(Photo Credit: Jeff Fitlow/Rice University)
"This ratio proved to be a robust marker for prognosis," said MD Anderson co-author Anil Sood, professor of gynecologic oncology and reproductive medicine and co-director of the Center for RNA Interference and Non-Coding RNA. "A high ratio was directly correlated to tumor aggression and metastatic capability. Patients with this profile had the worst prognosis for survival."
The three-year study included cell culture studies at Rice as well as a detailed analysis of gene-expression profiles of more than 500 patients from the Cancer Genome Atlas and protein-expression profiles from about 200 MD Anderson patients.
"The enzyme glutaminase is key to glutamine uptake from outside the cell, and glutaminase is the primary target that everybody is thinking about right now in developing drugs," Nagrath said. "We found that targeting only glutaminase will miss the less aggressive ovarian cancer cells because they are at a metabolic stage where they are not yet glutamine-dependent."
Rice graduate student Lifeng Yang, lead author of the study, designed a preclinical experiment to test the feasibility of a multidrug approach. He used a drug to inhibit the early stage production of internal glutamine while also limiting the uptake of external glutamine.
"That depleted all sources of glutamine for the cells, and we found that cell proliferation decreased significantly," Yang said.
Nagrath said the study also revealed another key finding -- a direct relationship between glutamine and an ovarian cancer biomarker called STAT3.
"A systems-level understanding of the interactions between metabolism and signaling is vital to developing novel strategies to tackle cancer," said MD Anderson co-author Prahlad Ram, associate professor of systems biology and co-director of the MD Anderson Cancer Center's Systems Biology Program. "STAT3 is the primary marker that is used today to ascertain malignancy, tumor aggression and metastasis in ovarian cancer."
Nagrath said, "The higher STAT3 is, the more aggressive the cancer. For the first time, we were able to show how glutamine regulates STAT3 expression through a well-known metabolic pathway called the TCA cycle, which is also known as the Krebs cycle."
Nagrath said the research is ongoing. Ultimately, he hopes the investigations will lead to new treatment regimens for cancer as well as a better understanding of the role of cancer-cell metabolism in metastasis and drug resistance.
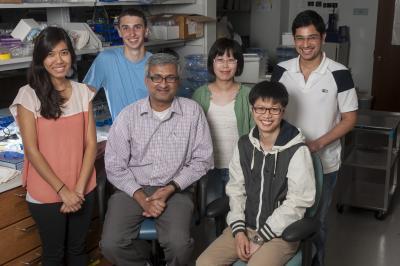
Researchers at Rice University's Laboratory for Systems Biology of Human Diseases analyzed the metabolic profiles of hundreds of ovarian tumors and discovered a new test to determine whether ovarian cancer cells have the potential to metastasize. Study co-authors include, from left, Julia Win, Stephen Wahlig, Deepak Nagrath, Hongyun Zhao, Lifeng Yang and Abhinav Achreja.
(Photo Credit: Jeff Fitlow/Rice University)
Source: Rice University