Examining 12 major types of cancer, scientists at Washington University School of Medicine in St. Louis have identified 127 repeatedly mutated genes that appear to drive the development and progression of a range of tumors in the body. The discovery sets the stage for devising new diagnostic tools and more personalized cancer treatments.
The research, published Oct. 17 in Nature, shows that some of the same genes commonly mutated in certain cancers also occur in seemingly unrelated tumors. For example, a gene mutated in 25 percent of leukemia cases in the study also was found in tumors of the breast, rectum, head and neck, kidney, lung, ovary and uterus.
Based on the findings, the researchers envision that a single test that surveys errors in a swath of cancer genes eventually could become part of the standard diagnostic workup for most cancers. Results of such testing could guide treatment decisions for patients based on the unique genetic signatures of their tumors.
New insights into cancer are possible because of advances in genome sequencing that enable scientists to analyze the DNA of cancer cells on a scale that is much faster and less expensive today than even a few years ago. While earlier genome studies typically have focused on individual tumor types, the current research is one of the first to look across many different types of cancer.
"This is just the beginning," said senior author Li Ding, PhD, of The Genome Institute at Washington University. "Many oncologists and scientists have wondered whether it's possible to come up with a complete list of cancer genes responsible for all human cancers. I think we're getting closer to that."
The new research analyzed the genes from 3,281 tumors – a collection of cancers of the breast, uterus, head and neck, colon and rectum, bladder, kidney, ovary, lung, brain and blood. In addition to finding common links among genes in different cancers, the researchers also identified a number of mutations exclusive to particular cancer types.
Looking at a large number of tumors across many different cancers gives the researchers the statistical power they need to identify significantly mutated genes. These genetic errors occur frequently in some cancers and rarely in others but are nevertheless thought to be important to cancer growth. The research was conducted as part of The Cancer Genome Atlas Pan-Cancer effort, funded by the National Cancer Institute and the National Human Genome Research Institute, both at the National Institutes of Health (NIH).
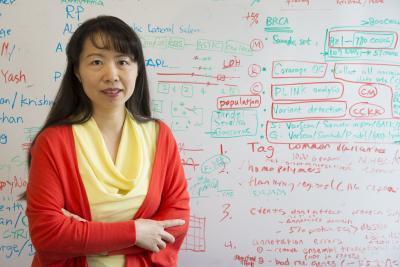
By analyzing the DNA in more than 3,000 tumors, scientists led by Li Ding, PhD, at The Genome Institute have identified 127 repeatedly mutated genes that likely drive the growth of a range of cancers in the body. The discovery sets the stage for devising new diagnostic tools and more personalized cancer treatments aimed at the unique genetic changes found in individual tumors.
(Photo Credit: Robert Boston, Washington University in St. Louis)
While the average number of mutated genes in tumors varied among the cancer types, most tumors had only two to six mutations in genes that drive cancer. This may be one reason why cancer is so common, the researchers said. "While cells in the body continually accumulate new mutations over the years, it only takes a few mutations in key driver genes to transform a healthy cell into a cancer cell," noted Ding.
The scientists, which included co-first authors Cyriac Kandoth, PhD, and Michael McLellan, both at Washington University, along with collaborator Benjamin Raphael, PhD, from Brown University, were also able to identify genes that have a significant effect on survival.
TP53, an already well-known cancer gene, occurred most commonly across the different tumor types. It was found in 42 percent of samples and routinely was associated with a poor prognosis, particularly in kidney cancer, head and neck cancer and acute myeloid leukemia.
Another gene, BAP1, also was linked with an unfavorable prognosis, especially in patients with kidney and uterine cancer.
However, mutations in the breast cancer gene BRCA2 were associated with improved survival in ovarian cancer, while errors in IDH1 were linked to an improved prognosis in gliobastoma, a particularly aggressive brain tumor, and in other cancer types.
Research to find additional cancer genes is ongoing at Washington University's Genome Institute, one of the large-scale genome sequencing centers supported by NIH, and at other academic institutions. Identifying a more comprehensive list of cancer genes could provide the backdrop to improve the diagnosis of cancer and to guide treatment decisions.
"Because we now know, for example, that genes mutated in leukemia also can be altered in breast cancer and that genetic errors in lung cancer also can show up in colon and rectal cancer, we think one inclusive diagnostic test that includes all cancer genes would be ideal," Ding said. "This would provide a more complete picture of what's going on in a tumor, and that information could be used to make decisions about treatment."