The European Perinatal Health Report released by the EURO-PERISTAT project is the most comprehensive report on the health and care of pregnant women and babies in Europe and brings together data from 2010 from 26 European Union member states, plus Iceland, Norway and Switzerland. EURO-PERISTAT takes a new approach to health reporting. Rather than simply comparing countries on single indicators such as infant mortality, our report paints a fuller picture by presenting data about mortality, low birthweight and preterm birth alongside data about health care and maternal characteristics that can affect the outcome of pregnancy. It also illustrates differences in the ways that data are collected and explains how these can affect comparisons between countries.
The first EURO-PERISTAT report, with data for 2004, was published in 2008. It found wide differences between the countries of Europe in indicators of perinatal health and care. Documenting these differences is important because it shows that gains are possible in most countries, provides information about alternative ways of providing care, and raises important questions about the effectiveness of national healthcare policies and the role of evidence in maternity care. This second report provides the opportunity to see whether these gains have been achieved and whether inequalities between the countries of Europe have narrowed.
The 250-page European Perinatal Health Report is a major feat of collaboration between researchers and official statisticians in Europe. It also contains data from two other European projects: Surveillance of Cerebral Palsy in Europe (SCPE) and European Surveillance of Congenital Anomalies (EUROCAT).The EURO-PERISTAT project is cofinanced by the Health Programme of the European Union's Directorate General for Health and Consumers which also provides funding for SCPE and EUROCAT.
REPORT HIGHLIGHTS
HEALTH OUTCOMES
Preterm birth rates stayed the same or declined in many countries. Previous reports, including a new study issued by the EURO-PERISTAT group (see below) have found increases in overall preterm birth rates over the past 15 years. In contrast, our data for 2010 suggest that increases may have stopped in some countries. Understanding why these rates have stabilised or decreased in some countries can help shape health policies in countries where rates continue to rise.
European congenital anomaly registries (in the EUROCAT network) recorded a total prevalence of major congenital anomalies of 25.5 per 1000 births for 2006-2010. The prevalence among live births was 20.9 per 1000 births. Extrapolating to the EU-27, this represents approximately 112 000 affected live births. Although most fetuses affected by a congenital anomaly survive the first year of life, these anomalies are a major contributor to fetal and neonatal deaths. The total perinatal mortality rate associated with congenital anomaly was 0.81 per 1000 births. Rates of termination of pregnancy for fetal anomaly varied between regions and countries from 0 to 10.5 per 1000 births. The decade through 2010 saw shallow declines in the prevalence of non-chromosomal anomalies including neural tube defects and congenital heart defects and an increase in some congenital anomalies including Down syndrome and Gastroschisis.
Cerebral palsy affects one newborn in 500 per year. Population-based registries across Europe have shown a decrease in cerebral palsy rates in children born with very low birth weight or moderate gestational age.
Maternal deaths are rare in Europe, but under-reporting is widespread. The maternal mortality ratio (MMR) ranges from under 3 per 100 000 (in Estonia, Italy, Austria, and Poland) to over 10 per 100 000 live births (Latvia, Hungary, Slovenia, Slovakia, and Romania). Although considerable variation arises from the very small numbers of deaths involved, there is good evidence that maternal deaths derived from routine statistical systems are under-reported. This must be investigated particularly for countries where ratios are very low.
CHARACTERISTICS OF CHILDBEARING WOMEN
Some risk factors for poor perinatal outcome increased, while others decreased. Levels of risk vary greatly between countries.
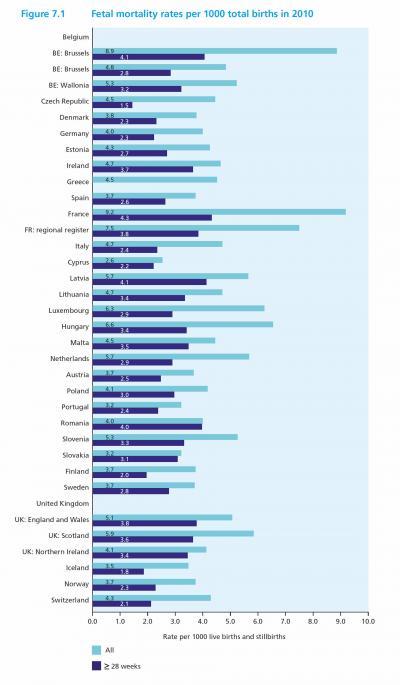
Fetal mortality rates at or after 28 weeks of gestation ranged from under 2.0 per 1000 live births and stillbirths in the Czech Republic and Iceland to 4.0 or more per 1000 in France, Latvia, the region of Brussels in Belgium, and Romania. The countries of the United Kingdom also had relatively high fetal mortality rates.
(Photo Credit: Euro-peristat/Inserm)
HEALTH SERVICES
Caesarean section rates increased in most countries between 2004 and 2010. With the exception of Finland and Sweden, where rates declined, increases were widespread ranging from under 0.2% in Italy to over 7% in Lithuania, Slovakia, and Poland. In general, increases were most marked in the countries of central and eastern Europe and in Germany and Austria.
Practices related to caesarean section have not converged over time. Rates in 2010 ranged from 52.2% in Cyprus, 38.0% in Italy, 36.9% in Romania and 36.3% in Portugal to below 20% in the Netherlands, Slovenia, Finland, Sweden, Iceland, and Norway. Differences in population risk factors for caesarean section, such as maternal age and parity do not suffice to explain these wide differences. Among countries with high proportions of older mothers Italy and Portugal had high caesarean section rates while the Netherlands and Finland had lower rates.
Variations in obstetric practices raise questions about the role of scientific evidence in clinical decision making. In addition to caesarean, other aspects of clinical practice also varied widely. For example, episiotomy rates ranged from 5% to 70% of vaginal deliveries, yet current evidence does not support routine use of this procedure. Rates were around 70% in Cyprus, Poland, Portugal, and Romania and ranged from 43-58% in Wallonia and Flanders in Belgium and in Spain. The lowest rates - between 5 and 7% - were reported in Denmark, Sweden, and Iceland.
Up to 5 to 6% of births in some countries may occur after use of some form of assisted reproductive techniques (ART), although the use of the less invasive procedures is under-reported in most data systems or not reported at all. Births after in vitro fertilisation (IVF) accounted for 2 to 4% of all births. Many countries are implementing policies to prevent multiple pregnancies in assisted conception, and the decrease in twin rates observed in some countries – such as Denmark, the Netherlands and Norway – may be the result of these policies. In contrast, the substantial increases in twin birth rates observed in Italy, Malta, Luxembourg, Brussels in Belgium and the Czech Republic could result from more widespread use of ART without clear practice guidelines.
While the proportion of births in larger maternity units has increased in many countries, the size of maternity units still varies widely. Overall, few births occurred in maternity units with fewer than 500 births in 2010, but this proportion was higher in some countries (16.1% in Germany, 17.6% in Estonia, 18.3% in Switzerland, and 61.9% in Cyprus). At the other end of the spectrum, in Denmark, Ireland, Latvia, Slovenia, Sweden, England and Scotland, over one quarter of births take place in maternity units with 5000 or more deliveries per year.
THE FUTURE OF PERINATAL HEALTH REPORTING IN EUROPE
European countries face common challenges related to the health and care of mothers and babies as shown by the results of this and the previous EURO-PERISTAT report. By making its perinatal health indicators widely available to health planners, clinicians, researchers and users, EURO-PERISTAT seeks to promote evidence-based actions to improve maternal and child health. Yet to build a truly sustainable system, further actions are needed to:
Improve national capacity for perinatal health reporting by ensuring that each country can provide the full set of EURO-PERISTAT indicators using appropriate definitions as well as by improving ascertainment of very preterm births and maternal deaths. Wider linkage of data sources, building on methods already in use in Europe, could yield immediate gains for perinatal health monitoring in many countries.
Reinforce European collaborations to produce and use these data. The EURO-PERISTAT network has published 20 articles in peer-reviewed journals based on these data. Other researchers have also used the EURO-PERISTAT data for research on perinatal health in their own countries. We expect that these new data from 2010 – which allow exploration of time trends in maternal and infant health–to further highlight the value of having comparable data from the countries in Europe.
Source: INSERM (Institut national de la santé et de la recherche médicale)