"Patients with PAD experience foot pain, called 'claudication,' while walking," adds Gautam Shrikhande, M.D., assistant professor of surgery, and director of the Vascular Laboratory at Columbia's Medical Center. "This pain continues, even at rest, as the disease progresses. In more advanced stages, PAD patients develop sores or ulcers that won't heal. Then, cell death, a.k.a. 'gangrene,' occurs and amputation is often the only solution. It's extremely important to diagnose PAD early, because medication and lifestyle changes can alleviate the disease."
This is where DDOT can help. "We've successfully used DDOT to detect PAD in the lower extremities," says Michael Khalil, a Ph.D. candidate working with Hielscher at Columbia. "One key reason why DDOT shows so much promise as a diagnostic and monitoring tool is that, unlike other methods, it can provide maps of oxy, deoxy and total hemoglobin concentration throughout the foot and identify problematic regions that require intervention."
"Using instrumentation for fast image acquisition lets us observe blood volume over time in response to stimulus such as a pressure cuff occlusion or blockage," said Hielscher.
To map and monitor the presence of hemoglobin, the protein that carries oxygen in the blood, red and near-infrared light is shone at different angles around areas that are susceptible to arterial disease. These specific wavelengths of light are then absorbed or scattered, depending on the concentration of hemoglobin.
"In the case of tissue, light is absorbed by hemoglobin. Since hemoglobin is the main protein in blood, we can image blood concentrations within the foot without using a contrast agent," Hielscher points out. Contrast agents pose the risk of renal failure in some cases, so the ability to monitor PAD without using a contrast agent is a great advantage.
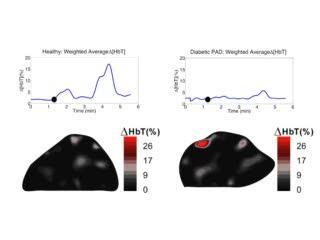
This movie compares the blood flow dynamics in a cross-section of the foot between a healthy individual and a diabetic patient with PAD. Differences are clearly visible in both the amplitude and speed at which the blood reacts to two applications of a pressure cuff (60 and 120 mmHg) around the thigh.
(Photo Credit: Andreas Hielscher, Columbia University.)
Since more than 25 million people — or 8 percent of the population — in the United States are diabetic, this diagnostic tool has the potential to make it significantly simpler to diagnose and monitor diabetics with PAD in the future.
Khalil, Hielscher, and colleagues hope to bring their diagnostic tool to market and into clinics within the next 3 years.
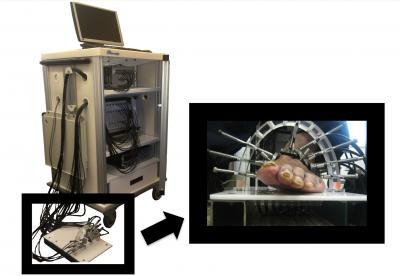
This shows a dynamic diffuse optical tomography system and the measurement probe.
(Photo Credit: Biomedical Optics Express.)
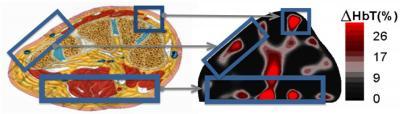
The locations of hemoglobin change within the 2D reconstructions correlate with the expected anatomy of the cross section of the foot.
(Photo Credit: Biomedical Optics Express.)
Source: Optical Society of America