A combination of genetic predisposition and environmental factors is believed to cause autoimmune (type 1) diabetes. A study published on March 27th in PLOS Pathogens gets at the mechanisms by which rotavirus infection contributes to autoimmune diabetes in a mouse model of the disease.
NOD (for non-obese diabetic) mice are prone to develop diabetes, and infection with rotavirus accelerates onset of the disease. Barbara Coulson and colleagues, from The University of Melbourne, Australia, tested the hypothesis that the virus does this by inducing "bystander activation".
Bystander activation assumes that a foreign intruder (in this case rotavirus) provokes a strong but non-specific activation of the immune system, and that this heightened state of activation "spills over" to a subset of specific immune cells that can recognize and attack not the viral intruder but some of the body's own cells, in this case the insulin-producing islet cells in the pancreas.
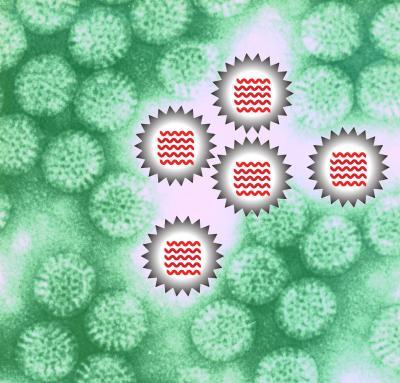
This is a cartoon of rotavirus particles (gray) containing their genome (red) on a background of real rotavirus particles imaged by electron microscopy (green). The rotavirus genome is detected by the immune response. This leads to increased activity of immune cells that possess the potential to destroy pancreatic islets.
(Photo Credit: Barbara Coulson, et al.)
Indeed, the researchers found that when spleen cells from NOD mice encounter rotavirus, they activate two types of immune cells: antibody-producing B cells and so-called dendritic cells that are a key part of a coordinated immune response. They could show that this activation involves "unpacking" of the virus (thereby exposing its viral immune activators), as well as specific immune mediators of the host, including one called TLR7 and type 1 interferons.
Rotavirus activation of a specific dendritic cell type called plasmacytoid dendritic cells was necessary for activation of another type of immune cells called T cells. These T cells can recognize and destroy islet cells and are ultimately responsible for type 1 diabetes. When activated, plasmacytoid dendritic cells produce very high levels of type 1 interferons, suggesting it has a specific role in mediating the bystander effect that connects rotavirus infection to accelerated diabetes.
Taken together, the results suggest that viral infection is capable of accelerating type 1 diabetes through an immune bystander effect and points to a number of key players--immune cells and immune modulators like interferon--that are linked to disease acceleration in the mouse model and worth investigating in humans. The authors conclude that, in particular, "the role of type 1 interferon signaling in diabetes acceleration following rotavirus infection deserves further analysis."
Source: PLOS